
The rabies vaccine is a preventive measure that protects against the rabies virus, a fatal disease that affects the central nervous system. This vaccine stimulates the immune system to produce antibodies, which prepares the body to fight the virus if exposure occurs.
Rabies is a disease primarily transmitted through the bite or scratch of an infected animal, most commonly dogs, bats, raccoons, foxes, and other mammals. Once symptoms appear, the disease is almost always fatal, which makes vaccination crucial for individuals at risk of exposure.
The rabies vaccine is administered in two primary contexts: pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP).
The rabies vaccine is highly effective when administered promptly and correctly. It plays a crucial role in preventing a disease that remains a significant public health concern in many parts of the world.
The rabies vaccine works by stimulating the immune system to recognise and respond to the rabies virus before it can cause a fatal infection. It contains inactivated (killed) rabies virus, which cannot cause the disease but effectively triggers an immune response.
Once administered, the vaccine prompts the body to produce rabies virus-specific antibodies. These antibodies remain in the bloodstream and act as the body’s defence mechanism, which neutralises the virus if exposure occurs. The vaccine also helps train immune cells, particularly memory B cells, to recognise and attack the virus more efficiently in future encounters.
The vaccine is used in two different contexts—pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP)—each working in a specific way:
It’s important to note that protection is long-lasting but not permanent. Boosters may be needed for those at continued risk of exposure. For post-exposure cases, a full PEP regimen is necessary to ensure complete protection.
Rabies vaccines are not mandatory for the general public in Singapore, as the country is classified as rabies-free and maintains strict animal import controls to prevent the introduction of the virus.
However, vaccination may be required or strongly recommended for specific groups based on risk level:
While not part of routine immunisation in Singapore, the rabies vaccine remains a critical safeguard for those with potential exposure risks, both locally and abroad.
The rabies vaccine is a life-saving preventive measure that offers protection against a disease with nearly a 100% fatality rate once symptoms develop. Key benefits of the rabies vaccine include:
By preventing the spread of rabies and ensuring early protection, the rabies vaccine remains one of the most effective tools in global rabies prevention.

The rabies vaccine is generally safe and well-tolerated, with millions of doses administered worldwide each year. Like any vaccine, it may cause mild side effects, but serious reactions are rare. The benefits of vaccination far outweigh the risks, especially considering that rabies is almost always fatal once symptoms appear.
Most people experience only mild and temporary reactions, which typically resolve on their own within a few days. These may include:
Immediate medical attention should be sought if any of the following symptoms develop:
While the rabies vaccine is safe for most individuals, the following groups of people should consult a doctor before receiving it:
Singapore is officially rabies-free, with strict regulations in place to prevent the introduction of the virus. However, certain individuals may still need the rabies vaccine due to travel, occupational risks, or potential exposure to animals imported from rabies-endemic regions. High-risk groups who should consider vaccination includes:
The rabies vaccine is administered in two key situations: pre-exposure prophylaxis (PrEP) for individuals at risk of rabies exposure and post-exposure prophylaxis (PEP) for those who have been bitten, scratched, or exposed to potentially rabid animals. The timing and dosage depend on the purpose of vaccination.
| Type of Prophylaxis | Who Needs It | Schedule | Additional Notes |
| Pre-Exposure Prophylaxis (PrEP) | Individuals at higher risk — travellers to endemic areas, veterinarians, animal handlers. | Primary series: 3 doses on days 0, 7, and 21 or 28. | Booster every 2–3 years for those at ongoing risk or as advised by antibody testing. |
| Post-Exposure Prophylaxis (PEP) | Individuals bitten, scratched, or exposed to potentially rabid animal saliva. | Depends on the vaccination history. | Immediate medical attention is essential. |
| Unvaccinated individuals | 4 doses — days 0, 3, 7, and 14. | RIG required on day 0 for deep wounds or high-risk exposure. | |
| Previously vaccinated individuals | 2 doses — days 0 and 3. | RIG is not required, as the immune system is already primed. |
The rabies vaccine is most effective when given as soon as possible after exposure. Delaying treatment increases the risk of the virus spreading to the nervous system, where it becomes fatal.
Rabies is a deadly disease with no cure once symptoms appear, which makes vaccination the most effective form of protection. Whether as a preventive measure for those at risk or an urgent treatment after potential exposure, the rabies vaccine plays a critical role in safeguarding lives. By stimulating the immune system to recognise and fight the virus, it provides essential protection against a disease that remains a global health concern.
At Phoenix Medical Group, your health and safety come first. Take the necessary steps to protect yourself and your loved ones by scheduling a consultation or vaccination appointment with us today.
How do I know if I need a rabies shot?
You may need a rabies shot if you have been bitten, scratched, or exposed to saliva from a potentially rabid animal. A healthcare provider can assess the risk and recommend vaccination.
Is 72 hours too late for a rabies vaccine?
No, 72 hours is not too late, post-exposure vaccination should still be started as soon as possible. It remains effective if administered within a few days of exposure.
How do I know if I have rabies?
Early symptoms may include fever, headache, and tingling at the wound site, followed by neurological signs like confusion or difficulty swallowing. Once symptoms appear, rabies is almost always fatal, seek medical help immediately after any potential exposure.
Can the rabies vaccine be administered alongside other vaccines or medications?
Yes, the rabies vaccine can generally be given with most other vaccines and medications without issues. However, individuals taking immunosuppressive drugs should consult a healthcare provider, as these medications might reduce the vaccine’s effectiveness.
Is the rabies vaccine safe for pregnant or breastfeeding women?
Yes, modern inactivated rabies vaccines are considered safe for both pregnant and breastfeeding women. They do not adversely affect fetal development or pose risks to breastfed infants.
What should I do if I miss a scheduled dose of the rabies vaccine?
If you miss a dose, contact your healthcare provider promptly. Minor deviations from the recommended schedule are generally acceptable, but it’s important to administer the missed dose as soon as possible to maintain protection.
Are there any dietary restrictions during rabies vaccination?
No, there are no scientific grounds for dietary restrictions during rabies vaccination. You can continue with your normal diet unless advised otherwise by your healthcare provider.
What should I do if I am bitten by an animal and my vaccination status is unknown?
Immediately wash the wound thoroughly with soap and water for at least 15 minutes. Seek medical attention promptly to assess the need for post-exposure prophylaxis, which may include the rabies vaccine and, if necessary, rabies immunoglobulin.
How effective is the rabies vaccine after exposure to the virus?
When administered promptly and correctly after exposure, the rabies vaccine is highly effective in preventing the onset of the disease. It’s crucial to begin treatment as soon as possible after a potential exposure.
Can animals other than dogs and cats receive the rabies vaccine?
Yes, rabies vaccines are also licensed for use in animals such as ferrets, cattle, horses, and sheep. Vaccination protocols may vary based on species and local regulations.
How can I reduce the risk of rabies exposure while traveling?
Avoid contact with wild or stray animals, ensure pets are vaccinated, and consider pre-exposure vaccination if traveling to areas where rabies is common. Consult your doctor or travel clinic for personalised advice before your trip.



9:00am to 8:30pm

9:00 am - 4:30 pm, 6.00 pm - 8:30 pm
9:00 am - 1:30 pm
2:00 pm - 8:30 pm

60 Paya Lebar Road, #02-09 Paya Lebar Square, Singapore 409051
9:00 am - 12:30 pm
2:00 pm - 5:00 pm
9:00 am - 12:30 pm

275 Thomson Road,
#01-05 Novena Regency,
Singapore 307645
9:00 am - 2:30 pm
6:00 pm - 8:30 pm (Mon, Tue, Wed & Fri)
9:00 am - 1:30 pm
2:00 pm - 8:30 pm
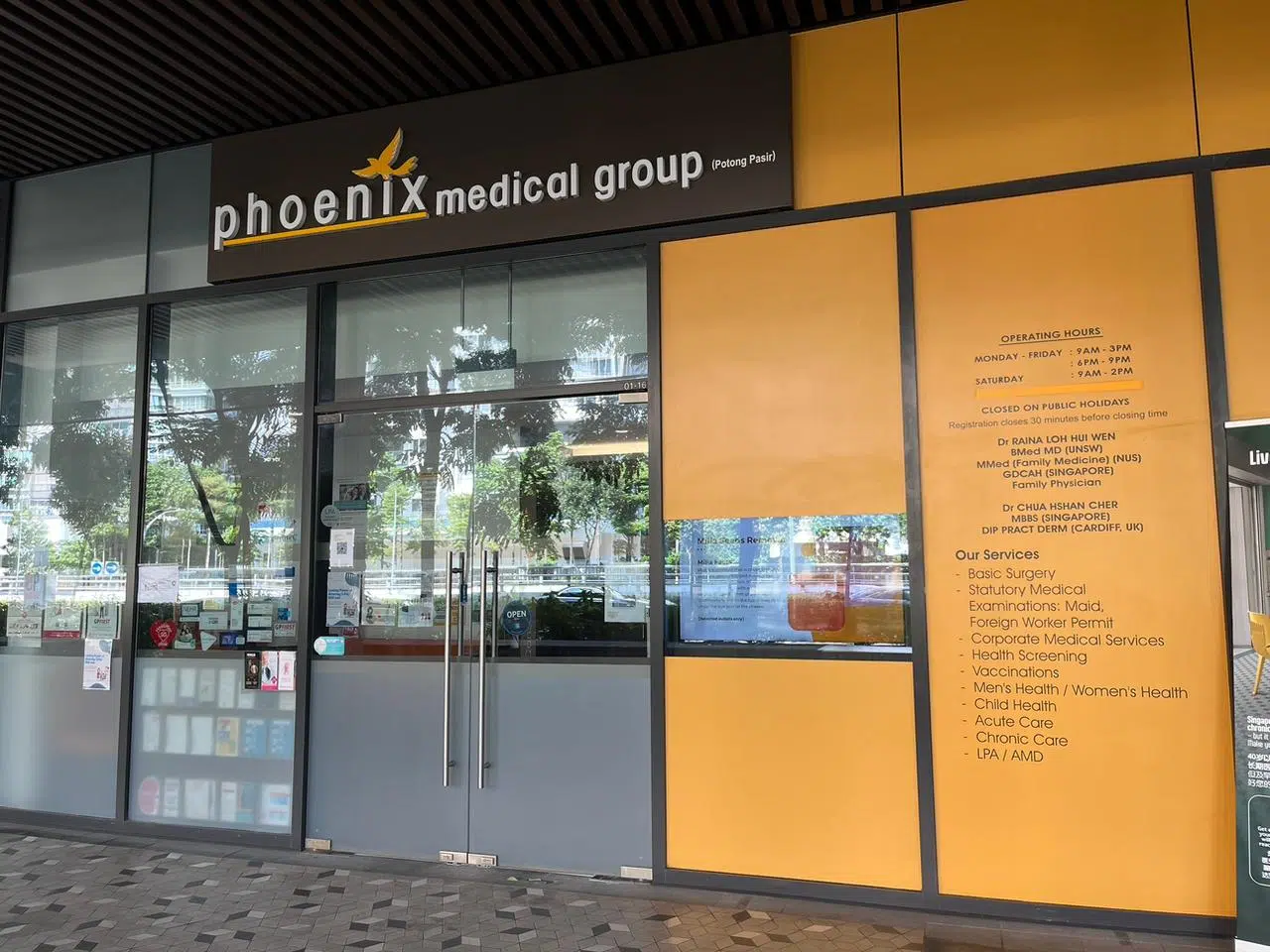
The Venue Shoppes,
2 Tai Thong Crescent, #01-16,
Singapore 347836
9:00 am - 3:00 pm
6:00 pm - 9:00 pm (Mon, Wed & Thu)
9:00 am - 2:00 pm
Closed

244M Upper Thomson Rd, Thomson Garden Estate, Singapore 574369
9:00 am - 3:00 pm
6:00 pm - 9:00 pm (Mon & Wed)
9:00 am - 2:00 pm
Closed

9:00 am - 4:00 pm
6:00 pm - 9:00 pm
9:00 am - 2:00 pm
Closed