
The Human Papillomavirus (HPV) vaccine is a proactive way to shield against infections caused by certain high-risk HPV strains. These strains are known to lead to various types of cancers, most notably cervical cancer. Additionally, the vaccine offers protection against cancers of the oropharynx, vulva, vagina, anus, and penis, as well as genital warts caused by specific HPV types.
Currently, three types of HPV vaccines are available:
Cervical cancer is primarily caused by persistent infections with high-risk HPV strains, particularly types 16 and 18, which are linked to approximately 70% of invasive cervical cancer cases in Singapore. As such, vaccination provides long-lasting protection, with studies showing high effectiveness for at least 12 years, and no signs of waning immunity.
Additionally, widespread HPV vaccination can reduce the global incidence of HPV-related cancers by up to 90%. This remarkable potential underscores its significance in safeguarding women’s health, particularly in countries like Singapore, where HPV-related cervical cancer remains a concern.
In fact, cervical cancer is the 10th most common cancer in Singapore, with approximately 429 new cervical cancers reported annually. The most common cervical cancer is squamous cell carcinoma, accounting for 80% to 85% of cases. Be that as it may, the incidence of cervical cancer has decreased in Singapore over the years due to Pap smear screening, early treatment of pre-invasive disease, and the increased awareness of the importance of the HPV vaccine.

The HPV vaccine leverages the immune system to identify, and defend against HPV infections. It contains virus-like particles (VLPs) that mimic the outer shell of the HPV virus but lack its genetic material, meaning it cannot cause an infection.
Upon vaccination, the immune system recognises these VLPs as a threat and generates antibodies targeting the HPV types included in the vaccine. This process also establishes immunological memory, enabling the immune system to rapidly respond to future HPV exposures, and prevent infection.
The vaccine is administered in a series of 2 or 3 doses, depending on the recipient's age. It is most effective when given before exposure to HPV, usually during adolescence. However, it can also benefit adults who have not yet been exposed to certain HPV strains, helping lower their risk of infection
The vaccination schedule varies by age:
To ensure optimal protection against HPV-related diseases, it is important to complete the entire series. If you miss a dose, there is no need to restart the series — simply consult your healthcare provider about when to get the next dose.
Although HPV is often associated with cervical cancer in women, men are also at risk of HPV-related health issues. Gardasil-9 is a powerful vaccine that protects against 9 HPV types linked to a variety of cancers, and conditions affecting men, including anal and penile cancer, oropharynx, as well as genital warts.
By receiving the HPV vaccine, men not only protect their own health, but also contribute to broader community immunity, reducing the overall transmission of the virus. Similarly, Gardasil-9 is recommended for boys, and men from age 9, and 26 years old, and may be considered for those aged 27, and 45 years old based on individual risk factors.
The HPV vaccine provides significant health advantages, including:
In addition to preventing cervical cancer, an HPV test provides valuable benefits such as detecting cervical cancer cells, identifying high-risk HPV strains, enabling early medical intervention, and monitoring overall reproductive health.
The HPV vaccine is generally well-tolerated, but some recipients may experience mild, short-term reactions, such as:
While these side effects are temporary, they are generally mild, and resolve on their own within a few days. Importantly, extensive studies have shown that there are no long-term health risks associated with the vaccine.

The HPV vaccine is primarily recommended for preteens, typically at ages 11 or 12, but it can be administered as early as age 9. Vaccinating at this early age is important because it provides protection before any potential exposure to HPV, which typically occurs through sexual contact. By vaccinating before exposure, the vaccine offers the highest level of effectiveness in preventing HPV-related diseases.
The vaccine is also recommended as a “catch-up” vaccination for teenagers, and young adults who did not receive it at the recommended age. However, this catch-up vaccination is typically recommended for individuals up to age 26.
For adults aged 27 through 46 who have not been vaccinated, the decision to get the HPV vaccine should be made in consultation with a doctor. While the vaccine is still effective in this age group, and can protect against new HPV infections, the likelihood of prior exposure may reduce its overall benefit.
However, for adults who are at risk of new HPV infections, such as those with multiple sexual partners or individuals who are not yet exposed to certain HPV types, the vaccine can still offer significant protection.
The HPV vaccine is a safe, and effective tool for most individuals, but there are specific situations where it is not recommended:

It goes without saying that the HPV vaccine is a critical tool in fighting against cervical cancer, and other HPV-related diseases. By preventing infections from high-risk strains of the HPV, the vaccine significantly reduces the risk of cervical cancer. Similarly, it helps protect against other types of cancer, and genital warts, which ultimately contributes to the overall public health.
At Phoenix Medical Group, we strongly encourage everyone, especially preteens, teenagers, and young adults, to get vaccinated as early as possible to ensure optimal protection. If you or a loved one are due for the HPV vaccine, schedule an appointment with us today.
Can the HPV vaccine be administered alongside other vaccines?
Yes, the HPV vaccine can be safely administered alongside other vaccines, such as the Tdap (tetanus, diphtheria, and pertussis), and meningococcal vaccines. This is typically done in a single visit for convenience, and to ensure comprehensive protection against various diseases.
Is the HPV vaccine mandatory for school attendance?
In Singapore, the HPV vaccine is not a requirement for school attendance. However, it is part of the national immunisation programme, and the Ministry of Health strongly recommends it for females aged 9 to 26 as a preventive measure against cervical cancer.
Can I still get the HPV vaccine if I am sexually active?
Yes, even if you are sexually active, the HPV vaccine can still protect you from strains of the virus that you have not been exposed to. It is recommended to discuss your individual situation with our doctors to determine if the vaccine is right for you.
Should women who have had the HPV vaccine still undergo regular Pap tests?
Yes, women who have received the HPV vaccine should continue adhering the recommended cervical cancer screening guidelines, including Pap tests. The vaccine does not protect against all high-risk HPV types, so screening remains an essential part of preventive healthcare.
Does the HPV vaccine offer any benefits to men?
Yes, men can benefit from the HPV vaccine. It helps protect against cancers of the throat, anus, and penis, as well as genital warts. Vaccinating men also helps prevent the spread of HPV to their partners, promoting better public health overall.
If I have had an HPV infection before, should I still get the vaccine?
This depends on your doctor’s assessment. Although the HPV vaccine cannot protect you from the specific strain you were previously infected with, it may protect you from other strains. It is important to consult with our doctors, as they can evaluate your individual situation, and provide guidance on the benefits of vaccination.
Is HPV similar to shingles?
No. HPV, and shingles are not the same. HPV is a group of viruses spread through skin-to-skin contact, often sexually, and can cause warts or, in some cases, cancers like cervical or throat cancer.
Shingles, on the other hand, are caused by the reactivation of the varicella-zoster virus (responsible for chickenpox), and cause a painful rash, typically affecting older adults or those with weakened immune systems.



9:00am to 8:30pm

9:00 am - 4:30 pm, 6.00 pm - 8:30 pm
9:00 am - 1:30 pm
2:00 pm - 8:30 pm

60 Paya Lebar Road, #02-09 Paya Lebar Square, Singapore 409051
9:00 am - 12:30 pm
2:00 pm - 5:00 pm
9:00 am - 12:30 pm

275 Thomson Road,
#01-05 Novena Regency,
Singapore 307645
9:00 am - 2:30 pm
6:00 pm - 8:30 pm (Mon, Tue, Wed & Fri)
9:00 am - 1:30 pm
2:00 pm - 8:30 pm
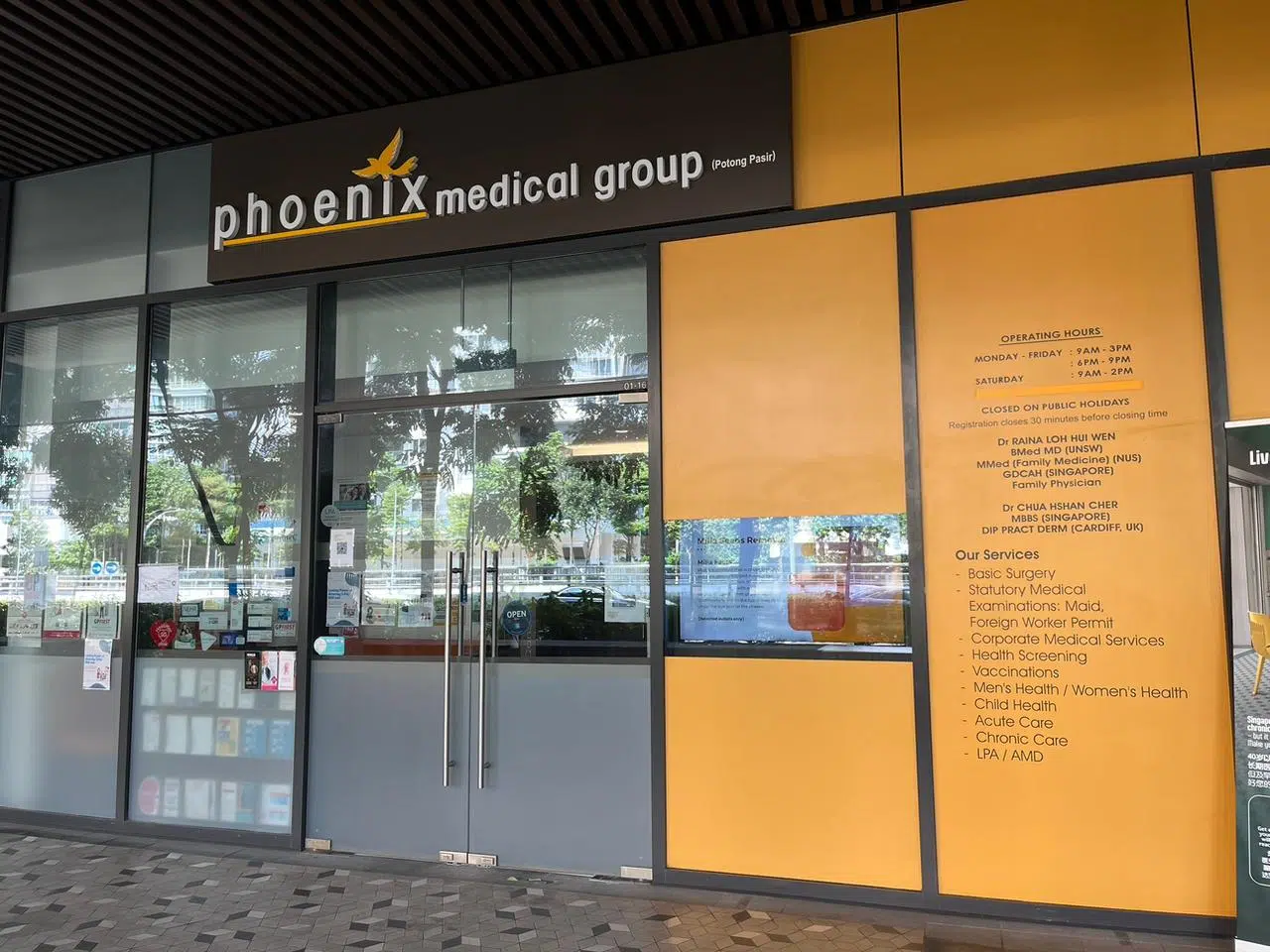
The Venue Shoppes,
2 Tai Thong Crescent, #01-16,
Singapore 347836
9:00 am - 3:00 pm
6:00 pm - 9:00 pm (Mon, Wed & Thu)
9:00 am - 2:00 pm
Closed

244M Upper Thomson Rd, Thomson Garden Estate, Singapore 574369
9:00 am - 3:00 pm
6:00 pm - 9:00 pm (Mon & Wed)
9:00 am - 2:00 pm
Closed

9:00 am - 4:00 pm
6:00 pm - 9:00 pm
9:00 am - 2:00 pm
Closed