
Diabetes is often described as a “silent” condition, one that develops gradually and, if unmanaged, can quietly cause lasting harm. Unlike an occasional skin breakout or a temporary flu, diabetes is long-term and requires daily attention. It does not just affect blood sugar levels, it can influence energy, mood, and even how well other organs function. Over time, poorly managed diabetes can lead to serious complications such as heart disease, kidney failure, nerve damage, and vision problems.
In Singapore, where lifestyle changes, urban stress, and diet patterns have contributed to rising diabetes rates, the condition has been described as a looming public health challenge. Yet, it is important to remember that with the right approach, diabetes is highly manageable. Effective care combines medical treatment, personalised lifestyle adjustments, and ongoing support. Many people living with diabetes lead full, active, and healthy lives when the condition is detected early and managed consistently.
The condition develops when the body cannot properly regulate blood sugar, and several contributing factors can set this in motion. While some risks are beyond our control, many are influenced by lifestyle, environment, and overall health.
These causes include:
Diabetes is not a single condition. It is a group of disorders that share one common feature: the body struggles to regulate blood glucose effectively. While type 1 and type 2 diabetes are the most widely recognised, several other forms are less common but equally important to understand.
The types of diabetes are:
Although the symptoms of these conditions may resemble those of type 1 or type 2 diabetes, less common forms often require specialist testing for accurate diagnosis. That is why consultation with an endocrinologist is recommended in complex or uncertain cases.
Both type 1 and type 2 diabetes lead to elevated blood sugar levels, but they develop for very different reasons. Some of the differences between the 2 conditions are:
| ASPECT | TYPE 1 DIABETES | TYPE 2 DIABETES |
| What is it? | An autoimmune disorder where the immune system attacks insulin-producing cells. | A progressive metabolic disorder characterised by insulin resistance and reduced insulin production over time. |
| Onset | Can occur at any age, but is most often diagnosed in children, teenagers, or young adults. | Can also occur at any age, but is more common in middle-aged and older adults. |
| Cause | Autoimmune destruction of pancreatic beta cells. | A combination of insulin resistance and a gradual decline in insulin production. |
| Insulin production | The pancreas produces little to no insulin. | The pancreas produces insulin, but the body may not respond effectively, or production decreases over time. |
| Prevalence | Less common, accounting for about 5 to 10% of all diabetes cases. | Much more common, making up around 90 to 95% of diabetes cases worldwide. |
| Treatment | Requires lifelong insulin therapy, alongside lifestyle and dietary management. | Managed with lifestyle changes, oral medication, and sometimes insulin if blood glucose remains uncontrolled. |
Living with diabetes affects far more than blood sugar levels. Because glucose is the body’s primary energy source, difficulty in regulating it can influence daily well-being, physical health, and even emotional resilience. People with diabetes may experience fluctuations in energy, frequent urination, constant thirst, and increased hunger, all of which can interfere with work, sleep, and daily routines.
Over time, the condition also places strain on mental health. The need for continuous monitoring, dietary adjustments, and regular medication can feel overwhelming, leading to anxiety or burnout. For some, visible consequences such as changes in weight, fatigue, or skin complications can affect self-confidence. Yet with the right management, many people can regain control, live actively, and reduce the long-term effects of the condition.
Uncontrolled diabetes can silently damage multiple organs and systems, often without noticeable warning signs in the early stages. Persistently high blood sugar weakens blood vessels and nerves, leading to complications that may only become evident after years. These can include:

Managing diabetes goes beyond controlling blood sugar. It requires a holistic approach that combines lifestyle changes, medication, and care for coexisting conditions. With the right strategies, most people with diabetes can lead active, fulfilling lives while lowering the risk of complications. Diabetes management typically involves:
A balanced diet plays a central role in managing diabetes. Paying attention to what you eat, how much you eat, and when you eat helps keep blood glucose levels steady throughout the day. Some dietary strategies that are often recommended include:
Physical activity helps the body use glucose more effectively, reduces insulin resistance, and supports cardiovascular health. Some tips to keep in mind:
For many people, diet and exercise alone are not enough to control blood sugar. Medications are commonly used to maintain glucose within a safe range. Your treatment will depend on the type of diabetes, your symptoms, and other health conditions. Some of the key considerations include:
Diabetes often goes hand in hand with other health issues. Addressing these conditions is an essential part of overall management:

At our primary care clinics, diabetes management is tailored to your needs and delivered by doctors experienced in long-term chronic care. The process is designed to help you take control of your condition while supporting your overall health and wellbeing.
It involves:
Many people only realise they have diabetes once symptoms appear — by then, the condition is already established. Prediabetes, on the other hand, often shows no warning signs at all, yet it significantly raises the risk of progressing to type 2 diabetes. This is why early detection and proactive management are so important.
You may benefit from regular screening and a structured diabetes management plan if you have one or more of the following risk factors:
Diabetes is a lifelong condition, but with the right care, it does not have to define your life. Understanding what causes it, recognising your risk factors, and taking steps to manage your health early can make all the difference in preventing complications. From healthy eating and regular exercise to medications and ongoing medical support, every part of diabetes management plays a role in helping you stay well.
Whether you have already been diagnosed, are at risk, or simply want peace of mind, a structured management programme offers the tools and guidance you need to take control of your health. By acting early, you can protect your long-term well-being and continue living a full, active, and confident life. Book an appointment with us to start your personalised diabetes management journey.
Type 2 diabetes can often be prevented or delayed with lifestyle changes. People with prediabetes may be able to reverse elevated blood sugar levels by eating a balanced diet, maintaining a healthy weight, and exercising regularly. If you are at risk, it is best to consult our doctor for a personalised prevention plan.
Diabetes does not disappear without treatment. While prediabetes can sometimes be reversed with proper lifestyle changes, once diabetes develops, it requires ongoing management. With consistent care, however, many people are able to achieve excellent control and reduce the risk of complications.
Common warning signs include frequent urination, excessive thirst, unexplained weight loss, and persistent fatigue. Women may also experience recurrent yeast infections. Since these symptoms can overlap with other health conditions, seeing a doctor for accurate testing and diagnosis is essential.
Yes. Stress triggers the release of hormones such as cortisol and adrenaline, which can cause blood sugar to rise. Prolonged stress may also contribute to insulin resistance, making diabetes harder to manage. Stress management techniques like mindfulness, exercise, or adequate rest can make a positive difference.
Medication should only be stopped if our doctor advises it, usually in cases where blood sugar levels are well controlled and remission has been achieved. Stopping medication suddenly without medical supervision can result in serious complications such as nerve or eye damage.
Diabetes is a lifelong condition, so most people will need to continue medication long term. In some cases, lifestyle changes can reduce the need for medication or allow dosages to be lowered, but this should always be discussed with your doctor.
No, eating sugar alone does not directly cause diabetes. Type 1 diabetes is an autoimmune condition unrelated to sugar intake. Type 2 diabetes develops due to a combination of genetics, lifestyle factors, and how the body processes insulin. That said, a diet high in sugar can contribute to weight gain, which is a risk factor for type 2 diabetes.
Having a family history of diabetes does increase your risk, especially for type 2 diabetes. However, lifestyle choices such as maintaining a healthy weight, exercising, and eating well can help delay or even prevent its onset, even in those with a genetic predisposition.
Yes. Type 1 diabetes is often diagnosed in children and young adults, while type 2 diabetes, once thought to affect mainly adults, is increasingly being seen in younger populations due to rising obesity rates. Early detection and treatment are key to protecting long-term health.



9:00am to 8:30pm

9:00 am - 4:30 pm, 6.00 pm - 8:30 pm
9:00 am - 1:30 pm
2:00 pm - 8:30 pm

60 Paya Lebar Road, #02-09 Paya Lebar Square, Singapore 409051
9:00 am - 12:30 pm
2:00 pm - 5:00 pm
9:00 am - 12:30 pm

275 Thomson Road,
#01-05 Novena Regency,
Singapore 307645
9:00 am - 2:30 pm
6:00 pm - 8:30 pm (Mon, Tue, Wed & Fri)
9:00 am - 1:30 pm
2:00 pm - 8:30 pm
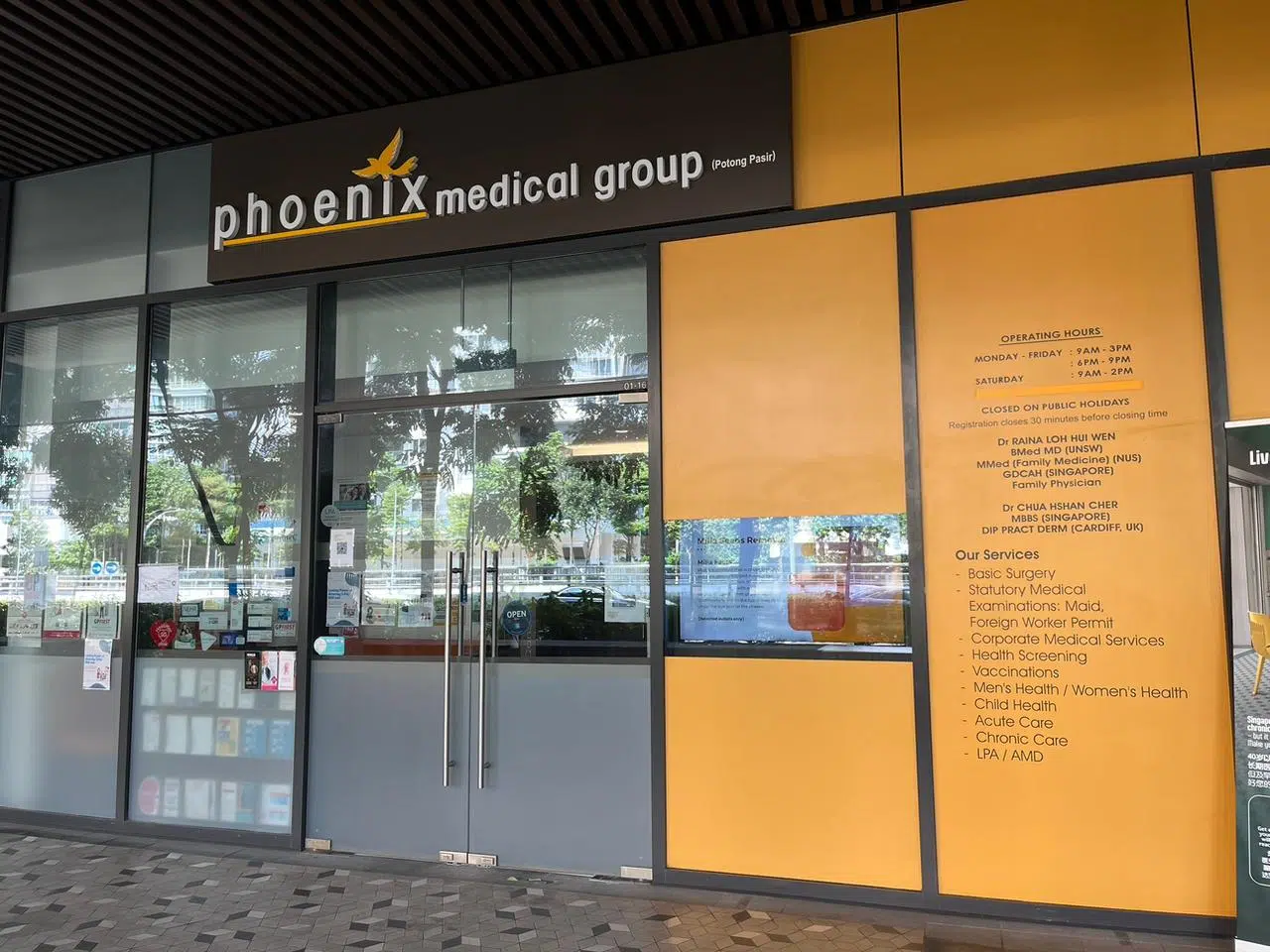
The Venue Shoppes,
2 Tai Thong Crescent, #01-16,
Singapore 347836
9:00 am - 3:00 pm
6:00 pm - 9:00 pm (Mon, Wed & Thu)
9:00 am - 2:00 pm
Closed

244M Upper Thomson Rd, Thomson Garden Estate, Singapore 574369
9:00 am - 3:00 pm
6:00 pm - 9:00 pm (Mon & Wed)
9:00 am - 2:00 pm

9:00 am - 4:00 pm
6:00 pm - 9:00 pm
9:00 am - 2:00 pm
Closed